Traumasoft Acquires Huly, Advancing a Market-First AI Strategy for the EMS Industry while Retaining Huly’s Market Independence
FOR IMMEDIATE RELEASE
Traumasoft Acquires Huly, Advancing a Market-First AI Strategy for the EMS Industry while Retaining Huly’s Market Independence
Portage, Michigan – January 29, 2026: Traumasoft, a leading provider of integrated EMS management solutions, is pleased to announce the acquisition of Huly, a specialized AI platform purpose-built to improve workflow efficiency, compliance, and staff experience across EMS operations. The acquisition reflects Traumasoft’s belief that AI is essential infrastructure for the EMS industry and must remain interoperable across the EMS ecosystem.
As part of the transaction, Huly will retain its independent brand, leadership team, and R&D engine to operate with meaningful autonomy under the ongoing direction of Founder and CEO Nidhish Dhru. This structure supports a market-first approach, allowing Huly to remain broadly accessible to EMS agencies regardless of their existing technology stack.
“This acquisition is about the future of EMS, not just the future of Traumasoft,” said Dave O’Reilly, CEO of Traumasoft. “We believe AI will become critical infrastructure for every EMS organization. Allowing Huly to operate with a degree of independence enables it to move quickly, stay market-focused, and deliver value across the entire EMS ecosystem, not just to Traumasoft customers.”
Investing in People: AI Built for the EMS Frontlines
The acquisition reinforces a shared belief that the most valuable asset in EMS is its people. Huly’s AI-powered tools are designed to reduce administrative burden, improve job satisfaction, and mitigate burnout, particularly in high-friction operational areas such as pre-billing, Quality Assurance / Quality Improvement (“QA / QI”), and payroll.
Agencies using Huly have reported:
- First-time billing rejections dropping from approximately 60% to near 10%
- Significant reductions in manual effort across pre-billing workflows
- Improved cash flow, accuracy, and staff productivity
“We built Huly to solve the real, often invisible problems that slow teams down and wear people out,” said Nidhish Dhru. “This partnership gives us the scale and resources to grow to better support our customers while staying focused on innovation and service to the fulsome EMS market.”
Largely Independent Structure, Shared Long-Term Vision
Traumasoft’s acquisition positions Huly as a market-first AI innovation engine built to serve the broader EMS ecosystem. Huly will operate with meaningful independence, maintaining control over its product roadmap and operating cadence, allowing it to move quickly and innovate on behalf of EMS providers industry-wide.
At the same time, Traumasoft customers will benefit from deep, tightly integrated workflows that connect HMS, billing, QA/QI, and AI-driven automation, delivering immediate and differentiated value within the Traumasoft platform.
This acquisition reflects Traumasoft’s long-term commitment to advancing EMS through scalable, industry-leading technology while ensuring its customers remain at the forefront of innovation.Shape
About Traumasoft
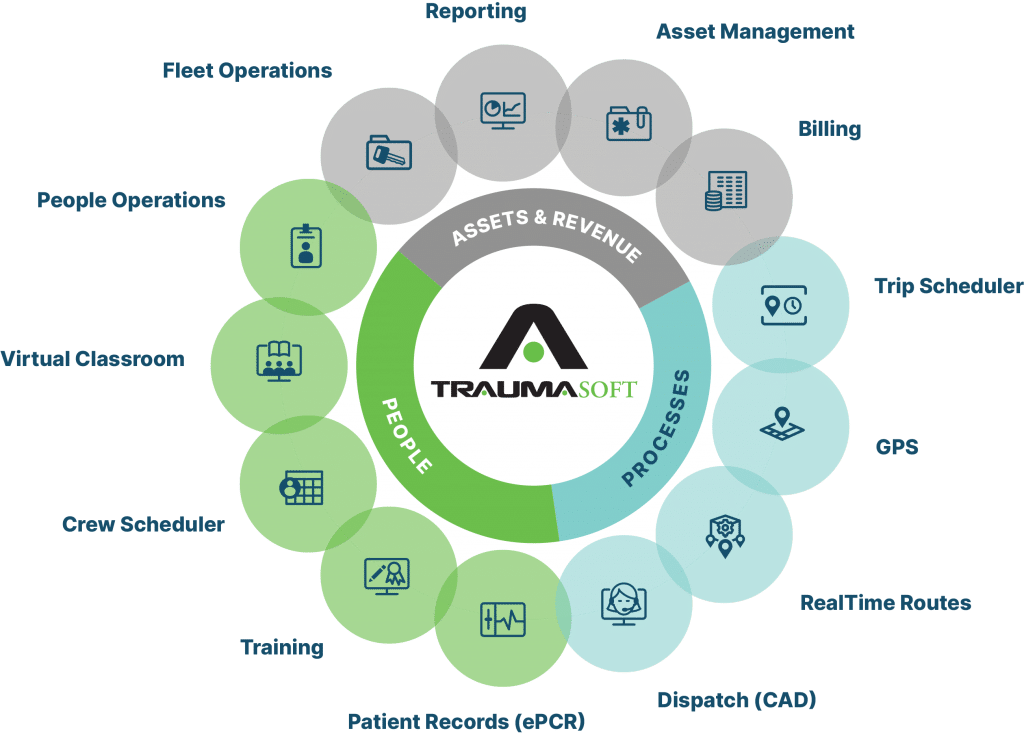
Traumasoft provides a comprehensive EMS operations platform designed to streamline scheduling, dispatch, ePCR, billing, fleet, and workforce management. The company is trusted by agencies across North America to simplify complexity, improve care coordination, and drive operational excellence.
About Huly
Huly is an AI-native platform built to enhance EMS agency workflows by automating time-intensive administrative processes. With a focus on revenue cycle management, QA/QI, and workforce operations, Huly delivers measurable gains in accuracy, efficiency, and scalability for EMS organizations of all sizes.
NEMT and Medicaid: Making it Work
What New Data Means for Transportation Providers
For years, Non-Emergency Medical Transportation (NEMT) has quietly helped Medicaid members get to the care they need. Recent federal reports and policy updates have pushed that role into the spotlight. Rather than being viewed as a side benefit, NEMT is increasingly recognized as a core part of how Medicaid delivers access, supports equity, and helps manage long-term costs.
Newer national data confirms that millions of Medicaid beneficiaries rely on NEMT each year to reach outpatient visits, behavioral health appointments, dialysis, and other recurring services. At the same time, transportation still represents a very small share of overall Medicaid spending. That combination—high impact, relatively low cost—is drawing more attention from policymakers and program leaders. They want to understand how NEMT is used, whether members are reaching care reliably, and how transportation connects to outcomes like avoidable emergency department use and hospitalizations.
Catching Up with the Industry
Policy has begun to catch up. Recent legislation explicitly codified NEMT as a required Medicaid benefit and directed federal agencies to take a closer look at how it’s delivered and overseen. Follow-up analyses have highlighted wide variation in state approaches: some rely on brokerage models, others lean on managed care organizations, and some use fee-for-service or hybrid structures. Across all of these models, themes keep emerging—stronger program integrity, clearer expectations around data and reporting, and a growing emphasis on health equity. States and plans want to be confident that trips are real, documented correctly, and reaching the members who need them most.
For NEMT providers, that translates into a shifting set of expectations. It’s no longer enough to simply complete trips; transportation partners are expected to provide reliable service, clean data, and insight into performance. That means being able to show on-time performance, no-show trends, and trip patterns across populations. It also means being prepared for audits and program integrity efforts, with documentation that holds up to scrutiny.
Meeting those expectations is challenging if operations are spread across multiple systems or managed manually. Traumasoft is designed to address that by bringing scheduling, dispatch, routing, GPS, fleet management, billing, and reporting into a single connected platform. When Trip Scheduler, Real-Time Routes, CAD, and GPS are all part of the same system, it becomes much easier to demonstrate reliability and efficiency. Facilities can submit trip requests online and see status updates in real time, while dispatchers can view live vehicle locations, crew status, and upcoming discharges through integrated tools like Bed Manager. Instead of relying on phone calls and manual logs, everyone sees the same, up-to-date information.
Reducing Guesswork
On the compliance and reporting side, integrated data reduces guesswork. Because trip details, routing, and billing all live within the same platform, NEMT providers can generate reports that answer the questions states and plans are asking: Who is using the benefit? How often? How reliably are trips being completed? Where are there gaps or delays? Built-in analytics help leaders monitor performance by contract, region, or payer, and catch potential issues before they become major problems.
These same tools support equity goals as well. When providers can see patterns across different populations and geographies, they can identify where transportation is working well and where access may be falling short. Over time, that kind of visibility makes it possible to collaborate more effectively with state agencies, brokers, and health plans on targeted improvements rather than just reacting to complaints or denials.
An Essential Part of the Continuum
At the end of the day, the new attention on NEMT confirms what providers already know: reliable transportation is an essential part of healthcare for many Medicaid members. The policy environment is simply making that reality more explicit—and more measurable. For NEMT operators, this creates both pressure and opportunity. There is pressure to meet higher standards for data, oversight, and performance. But there is also a real opportunity to stand out as a technology-forward, data-driven partner that makes it easier for states and plans to meet their own access, quality, and equity goals.
Traumasoft’s all-in-one EMS and NEMT platform is built to help providers make that shift. By unifying daily operations with the data needed for oversight and improvement, it gives NEMT organizations a foundation to adapt to changing expectations while continuing to deliver what matters most: dependable transportation to care for the people who need it.
EMS Workforce: Strength Through Retention
The EMS workforce is in the midst of a serious staffing crisis. Agencies across the country are facing high turnover, widespread burnout, and a shrinking pool of qualified candidates. While these challenges are steep, they also present an opportunity to rethink how we recruit, support, and retain EMS professionals for the long haul.
Short-term fixes aren’t enough. Recruitment and retention strategies must evolve into long-term, people-centered approaches. That means developing leaders who can build trust, communicate clearly, and help their teams manage stress constructively. EMS professionals need to feel seen, heard, and valued—not just for their skills, but for the service they provide.
“Retention starts at the top,” says Traumasoft Chief Sales Officer Joshua Porter. “When leaders are engaged and communication is clear, crews feel valued and want to stay.”
Real Investment in People Means Better Pay, Growth, and Support
Experts agree: improving retention starts with compensation and career support. Paramedics and EMTs work under intense pressure. Their pay and benefits should reflect the value they bring to communities.
Rather than offering one-time sign-on bonuses, agencies should focus on long-term investment in their people:
- Increase base pay and improve benefits for current staff
- Offer professional development and leadership training
- Create clear paths for advancement and career mobility
- Provide access to wellness programs and mental health services
- Encourage time off and limit excessive overtime
Burnout remains one of the leading reasons EMS professionals leave the field. Reducing emotional exhaustion requires both system-level changes and day-to-day support—from leadership, peers, and the tools used on the job.
EMS Workforce Recruitment Isn’t Reactive—It’s Strategic
One of the biggest missteps EMS agencies make is treating recruitment as a short-term fix. Instead, it should be an ongoing, strategic priority. Agencies can improve long-term recruitment by:
- Building partnerships with high schools, colleges, and training programs
- Offering early engagement opportunities like ride-alongs or internships
- Maintaining a visible, positive presence at career fairs and community events
- Demonstrating a clear career path beyond entry-level roles
Showing potential recruits that EMS is a long-term career—not just a stepping stone—can help attract the next generation of providers.
Technology as a Retention Tool
Modern EMS software solutions play an important role in workforce stability. From mobile access to automated scheduling and time tracking, digital platforms reduce administrative burdens and help employees focus on what matters most: patient care.
Traumasoft’s all-in-one EMS management platform is designed with the provider experience in mind. By streamlining workflows, improving transparency, and reducing stress, Traumasoft helps agencies operate more efficiently and retain the talent they already have.
“At Traumasoft, our mission is to help EMS agencies build environments where providers feel empowered, supported, and equipped to do their best work,” says Porter.
Supporting your team today is what builds a stronger EMS system tomorrow. A culture of respect, communication, and collaboration—paired with the right tools—lays the foundation for long-term success.
Ready to see how simple the switch to Traumasoft can be? Request a personalized migration roadmap today.
NEMT Plays Critical Role in Today’s Healthcare System

In today’s healthcare environment, access to care means more than being able to see a doctor—it also means ensuring patients can get to their appointments safely and on time. Non-Emergency Medical Transportation (NEMT) plays a crucial role in making that possible, especially for seniors, people with disabilities, those with lower incomes, and rural residents.
NEMT providers are essential in making healthcare more equitable and accessible. Missed medical appointments due to transportation barriers cost the U.S. healthcare system an estimated $150 billion annually. These costs include not only lost revenue for healthcare providers but also avoidable emergency care and hospital admissions—issues that could often be prevented with consistent outpatient care.
Why NEMT Matters—And Delivers Results
NEMT has a proven return on investment. On average, $268 is saved per user each year through reduced hospitalizations and emergency room visits. The impact is especially significant in rural and underserved urban areas, where public transportation may be limited or nonexistent. In these settings, NEMT ensures that individuals who might otherwise be cut off from care can still access vital health services.
Here’s what modern NEMT services make possible:
- Safe and timely transportation to medical appointments
- Fewer no-shows and improved care plan compliance
- Reduced reliance on emergency departments
- Increased patient satisfaction and continuity of care
How Technology is Transformational
Digital platforms are revolutionizing the way NEMT providers operate. Real-time ride tracking, automated scheduling, mobile documentation, and digital access all help improve both patient experience and operational efficiency. By reducing human error and improving accountability, digital tools ensure that patients are picked up and dropped off on time. This enables lower no-show rates and better overall outcomes.
At Traumasoft, our all-in-one EMS and NEMT platform is designed to reduce operational costs, streamline workflows, and enhance the patient experience. From smart scheduling and optimized routing to vehicle tracking and real-time reporting, we help providers meet growing demand without compromising care.
“We believe every missed appointment is a missed opportunity for better health,” says Traumasoft Chief Sales Officer Joshua Porter.. “That’s why our NEMT tools are designed to ensure patients get where they need to go—on time, every time.”
Looking Ahead: The Future of Healthcare Access
As healthcare systems face rising costs and growing demand for equitable care, NEMT will play an even more critical role in supporting public health. To maximize its impact, the industry needs broader support—through technology investment, workforce training, policy funding, and public education.
With more states and health plans going digital—and companies like Traumasoft leading the way—NEMT is poised for a leap forward.
“Getting to a doctor’s appointment shouldn’t be a barrier to staying healthy,” says Porter. “With the right tools in place, we can ensure everyone has access to the care they need.”
For healthcare providers, payers, and policymakers seeking to reduce costs and improve outcomes, technology-enabled NEMT must be part of the strategy. For millions of patients—especially those who are elderly, low-income, disabled, or living in underserved areas—reliable transportation is often the key to accessing routine care.
Without it, missed appointments, delayed treatments, and worsening health conditions become inevitable.
By connecting patients with care, NEMT providers prevent costly hospital visits, reduce healthcare spending, and improve long-term outcomes. Strengthening our healthcare system starts by recognizing NEMT as an essential part of patient care.
Ready to see how simple the switch to Traumasoft can be? Request a personalized migration roadmap today.
The EMS Workforce Crisis: Causes, Consequences, and the Path Forward
Emergency Medical Services (EMS) are the backbone of our healthcare system’s immediate response to crises. But today, EMS agencies across the country are facing a serious and growing workforce shortage—one that threatens the reliability and effectiveness of emergency care in communities nationwide.
Although EMS licensure numbers remain relatively stable, the number of active practitioners is steadily declining. More and more certified professionals are leaving the field, creating a critical staffing gap that is hard to fill.
Why EMS Professionals Are Leaving the Workforce
The reasons behind this shortage are complex and interconnected. Key drivers include burnout, low wages, limited career advancement, and lingering effects from the COVID-19 pandemic. Nearly 60% of EMS agencies report that they’re unable to meet 911 call demand—a clear signal that the system is under intense strain.
The result? Slower response times, increased workloads for remaining staff, and growing risks to both EMS professionals and the patients they serve.
Operational Tools That Ease the Burden
As an all-in-one EMS operations platform, Traumasoft is focused on helping providers stay efficient during this difficult time. From dispatch to billing, crew scheduling to real-time GPS tracking, every tool is designed to simplify operations and support the teams that deliver care.
“One of the biggest ways we help EMS teams is by giving them time back,” says Joshua Porter, Chief Sales Officer at Traumasoft. “That means automating the paperwork, simplifying communications, and giving crews tools they actually want to use.”
Key Factors Driving the EMS Workforce Shortage
- Burnout and Mental Health Challenges: EMS professionals face high-stress situations daily. The emotional toll—compounded by long shifts, traumatic calls, and pandemic-related demands—has led to widespread burnout.
- Compensation Concerns: EMS providers often earn significantly less than other healthcare professionals with comparable responsibilities. This wage gap makes it difficult to attract and retain qualified personnel.
- Limited Career Advancement: The lack of structured pathways for professional development discourages long-term commitment and leaves many EMS workers feeling stuck.
- Funding Cuts and Training Barriers: Reduced funding for EMS education and training programs has made it harder to grow the next generation of providers, further compounding the shortage.
How Traumasoft Supports EMS Resilience
The impact of the workforce shortage is already visible: increased response times, overburdened crews, and overextended healthcare systems. When EMS response slows, patient outcomes can suffer—and so can provider well-being.
Tackling this challenge will require bold steps, including improved compensation, clearer career paths, and better support systems for managing job-related stress. Traumasoft is tuned in to these issues and provides tools designed to help EMS organizations recruit and retain top-tier talent.
“We take seriously our role in helping EMS providers do more,” says Porter. “Our platform is built to make the workplace better for EMS professionals—by reducing burnout, improving operations, and allowing frontline teams to stay focused on what matters most: patient care.”
Moving Forward
There’s no sidestepping the fact that the EMS workforce shortage is a serious, systemic challenge. But by addressing the root causes and taking meaningful, coordinated steps, we can protect and strengthen this essential part of our healthcare infrastructure.
Ensuring the well-being of EMS professionals isn’t just a workforce issue—it’s a matter of public health and community safety.
Ready to see how simple the switch to Traumasoft can be? Request a personalized migration roadmap today.
The Most Asked Question at AAA: ‘How Hard is it to Switch to Traumasoft?’
The American Ambulance Association Conference & Trade Show in Lexington, Kentucky wrapped up this week, and our team left energized by the conversations we had at Booth 615. One question surfaced again and again: “Your platform is awesome, but how hard is it to switch to Traumasoft?”
The short answer: easier than you think. Below is a look at how Traumasoft makes onboarding smooth, fast, and stress-free.
Switch to Traumasoft: A Proven Onboarding Path
Most agencies moving to Traumasoft are fully operational within one to two weeks. Our Customer Success team maps out each phase—data migration, module set-up, user permissions, and go-live testing—so crews can keep answering calls while the platform comes online and you fully make the switch to Traumasoft.
Module-Based Training Built for EMS
Every Traumasoft deployment includes guided, role-specific training sessions. Using short, module-based lessons, supervisors and field staff learn exactly what they need—nothing more, nothing less—then practice on their own schedules. Continued refresher courses and an on-demand knowledge base keep skills sharp.
Three Reasons Agencies Call the Transition ‘Refreshingly Easy’
- Data comes with you. We handle imports from CAD, ePCR, billing, and HR systems—so historical records remain intact.
- One login, one interface. All modules live in a single, cohesive platform, eliminating the “patchwork” feel of bolt-on tools.
- Dedicated support after go-live. Our support team (many are former EMTs and paramedics) stays engaged long after launch, helping optimize workflows and reports as your needs evolve.
The bottom line: A modern EMS platform should remove friction, not add to it. By combining rapid onboarding, intuitive design, and ongoing training, Traumasoft lets agencies focus on what matters most—responding faster, caring better, and retaining great crews.
Ready to see how simple the switch to Traumasoft can be? Request a personalized migration roadmap today.
Problems with EMS Scheduling and How to Solve Them Using Technology

Emergency Medical Services (EMS) operate in a fast-paced environment where efficient scheduling is crucial to ensuring rapid response times and optimal patient care. However, traditional scheduling methods often lead to inefficiencies, staff burnout, and operational disruptions.
Fortunately, modern EMS scheduling software provides comprehensive solutions to these challenges. This article examines common EMS scheduling issues and how EMS solutions like Traumasoft can resolve them.
1. Staffing Inconsistencies and Scheduling Conflicts
Challenge: EMS schedules involve a mix of full-time, part-time, and on-call staff, making manual scheduling complex and error-prone. Mistakes such as understaffed shifts, double bookings, and last-minute conflicts can disrupt operations and delay response times.
Solution: EMS staff scheduling software automates the scheduling process, minimizing errors and improving workforce management. By considering factors like employee availability, certifications, and shift preferences, the software generates balanced schedules. Automated notifications keep staff informed, reducing no-shows and last-minute changes. Advanced algorithms also help identify and resolve conflicts before they arise.
2. Inefficient Shift Change Processes
Challenge: Shift changes are inevitable in EMS due to personal emergencies, illness, or other unforeseen circumstances. Traditional shift-change management involves excessive back-and-forth communication, leading to delays and scheduling conflicts.
Solution: Modern EMS scheduling systems include self-service portals where employees can request shift swaps or update their availability. Automated approval workflows streamline the process, reducing administrative overhead and ensuring seamless shift transitions.
3. Overtime Management and Staff Fatigue
Challenge: Overtime is common in EMS, often leading to employee exhaustion, increased turnover, and budget overruns. Manually tracking overtime can result in scheduling inefficiencies and excessive labor costs.
Solution: Scheduling software offers real-time tracking of staff hours, ensuring managers receive alerts when employees approach or exceed overtime limits. This helps maintain a balanced workload, preventing burnout while optimizing labor costs. By distributing shifts equitably, EMS organizations can promote employee well-being and operational efficiency.
4. Limited Access to Real-Time Data and Reports
Challenge: Manually generating reports and analyzing scheduling data is time-consuming and prone to errors. Without access to real-time insights, decision-makers struggle to optimize staffing levels and resource allocation.
Solution: EMS scheduling software should provide powerful reporting and analytics tools that deliver real-time insights into staffing trends, resource utilization, and shift attendance. Managers can generate detailed reports quickly, allowing for data-driven decision-making and continuous operational improvement.
5. Communication Gaps and Coordination Challenges
Challenge: Effective communication is essential for EMS operations, yet traditional methods can lead to miscommunication, delays, and inefficiencies. Coordinating shifts, notifying staff of updates, and managing last-minute changes can be cumbersome.
Solution: Many EMS scheduling solutions include integrated communication tools such as instant messaging and automated notifications. These features facilitate seamless coordination, ensuring that teams remain informed and aligned, ultimately improving response times and operational efficiency.
6. Inefficient Resource Allocation
Challenge: Poor resource allocation can delay critical care, affecting patient outcomes. Manual scheduling methods make it difficult to efficiently assign personnel, vehicles, and equipment, leading to wasted resources and inefficiencies.
Solution: EMS scheduling software optimizes resource allocation by strategically assigning personnel and assets based on real-time data. Integration with navigation tools allows for optimized routing, reducing travel time and fuel costs. By ensuring resources are used effectively, organizations can enhance response times and patient care.
Conclusion
Effective EMS scheduling is vital for maintaining operational efficiency and delivering high-quality patient care. Traditional scheduling methods often fall short, leading to staffing challenges and communication gaps. However, modern EMS scheduling software provides comprehensive solutions by automating key processes, improving team coordination, and offering valuable real-time insights.
2025 EMS Trends from 12 Industry Leaders
As 2025 unfolds, the EMS industry faces ongoing challenges like workforce shortages, financial pressures, and evolving healthcare demands. Yet, experts highlight transformative opportunities in areas such as artificial intelligence, data analytics, and community paramedicine programs.
Key trends include mental health support for providers, improved crisis communication, and adapting to regulatory changes under a new federal administration. With a focus on innovation, collaboration, and resilience, EMS leaders are shaping a future aimed at delivering high-quality, equitable care while navigating an ever-changing landscape.
Contributors
- Kevin E. Frisch. CEO, Banquest Payment Systems.
- Dale Loberger. MARVLIS Consultant, BCS; FTO, Union EMS; Chief at GRVFD.
- Greg Friese. Editorial Director, EMS1
- Scott Moore. Senior Consultant & Show Host, Moore EMS Consulting.
- Maggie Adams. President, EMS Financial Services.
- Chris Cebollero. President & CEO, Cebollero & Associates.
- Samuel Scheller. CEO, Guardian Elite Medical Services (NV).
- Nancy Magee. EMS Educator, consultant, conference speaker at MEDIC Training Solutions LLC.
- Mark Tenia. Public Relations/Media Manager, Richmond Ambulance Authority.
- Jim Karras. EMT, Principal of The Karras Group.
- Matt Koslosky. NEMT Transportation Solutions Expert.
- Omar Masri. CEO, Mamori.io.
1. Streamlining Payments for a Tech-Savvy Generation

Kevin E. Frisch
CEO, Banquest Payment Systems
The medical transportation industry is adapting to the needs of a more tech-savvy population that values convenience and immediacy in their financial interactions. Modern patients and their families increasingly prefer seamless payment methods that align with their everyday digital experiences—whether it’s a single-click transaction using stored payment methods or mobile-friendly options that eliminate the need for phone calls or emails. In response to this demand, we have collaborated with dozens of ambulance companies over the past year to fully integrate payment systems into their workflows. These efforts ensure that paying invoices is as effortless as possible, allowing patients and families to focus on care rather than administrative tasks.
2. Navigating Federal Policy Shifts and Their Impact on EMS

This could be an especially difficult year to forecast with a new federal administration looking to make significant changes, but the president-elect has been very clear about his policy priorities. Some of his promises relate to deregulation, spending cuts, and increased tariffs.
While the federal focus is not on EMS directly, healthcare in general will be targeted for some real changes. A general mood toward deregulation could allow for some new strategies of EMS delivery to be implemented. You can expect to see the trend of fire departments competing for contracts held by third-service EMS providers to continue with a promise to reduce local expenses. However, it is the spending cuts recommended for direct assistance programs that might have the most impact. We can anticipate a greater public dependence on EMS services with the possibility of less scheduled primary care being supported. Tariffs are also likely to have a direct effect on agencies by driving up the direct costs of many consumable expenses with many suppliers of goods being located outside of the US.
In general, it is also likely that rigid response time standards continue to lose their stranglehold on contract requirements. We are starting to see new criteria related to event outcomes beginning to replace a drive to just get to the scene quickly. With fewer federal dollars supporting EMS in reimbursements, it will be up to local governments to sustain EMS initiatives while we likely face increasing volume due to reductions in aid to poor families.
3. Overcoming Persistent Challenges to Elevate EMS Performance

The 2020s are half-over and EMS faces many of the same challenges it faced at the start of the decade – difficulty retaining high-performing field providers, too few people entering the career field and inadequate funding to provide reliable and high-quality service. Despite these headwinds, some high-performing EMS services are finding a way to reduce the risk of opioid overdose, transport patients to alternative care destinations and partner with law enforcement and mental health professionals to best serve those in mental health crisis. To join these top performers in 2025, all EMS agencies need to secure and stabilize their funding, collaborate or merge with neighboring agencies and inform their stakeholders of their successes and challenges.
4. A Year of Disruption in the Workplace

The new Presidential administration will bring with it significant changes in the workplace from a regulatory perspective. Over the last few years, we have seen significant action from both federal and state regulators. OSHA proposed the first update to rules impacting EMS and first responder agencies in 44 years. As we begin a new year and new administration, EMS leaders can expect dramatic changes in workplace oversight priorities. It will be critical that EMS leaders more deeply engage with their compliance efforts.
5. Strengthening Financial Practices and Compliance in EMS

EMS leaders will continue to look for opportunities to improve revenue and reduce costs. Going into 2025, treatment without transport coverage will grow as Medicaid plans recognize its value. I recommend investigating how to bill for these services. The new year will continue the need to meet the financial expectations of all levels of the workforce. Providers do not need the unexpected financial hit of a billing audit or a review of staff licensing requirements. My best advice for the coming year is for providers to check that their house is in order. We have the arrival of a new administration, and we do not yet know the impact (if any) on existing fraud and abuse oversight efforts – or if oversight will be expanded. Recent OIG work plan efforts affected both emergency and non-emergency providers. Therefore, take 2025 as an opportunity to clean up if necessary.
Outsourced billing continues to be a trend. It would be prudent for providers to look at billing (both Medicare and Medicaid). There has been consolidation and mergers among billing organizations. Whether billing in-house or outsourced, now is the time to audit documentation and billing for compliance. On another front, some organizations have had to pay back money because transports were performed by personnel whose credentials were not up to date. Ensure all staff credentials and training requirements are current so that no money needs to be paid back to third-party payers because a crew member was operating without proper licensure. The response to a government audit on any of these topics is costly and time-consuming. Look under the hood to see that all the issues that could potentially impact reimbursement or income are current. With assurance that financial matters are clean, providers will have more bandwidth to focus on operational and staffing issues that best support their communities.
6. The Role of AI in Shaping the Future of EMS

For the past few years there has been a certain amount of uncertainty in EMS. We are making strides to tackle those subjects which include reimbursement, recruiting, retention, and the MIH/CP transition. Even though we are making strides, they are slow going. Now we have a new fox in the henhouse and that is the booming use of AI in everything we do. What does the future of AI in EMS look like? I do not want to offer an answer, instead we need to now be anticipatory as to what we want to use AI for in EMS.
With just a shrug of the shoulder, initial and continuing education will make incredible strides in the AI universe. I was talking to a cardiologist friend of mine, and he just installed an AI documentation tool in his clinic. He walks into the room, begins his assessment and AI does all his documentation for him. Will this work in EMS? Let’s make it work in EMS. We have to remember that we are dependent on CMS for reimbursement, ensuring that our charts are completed correctly is a big deal. With all the trends in EMS, this is a great time to be happy and excited about the future. What does the future look like when it comes to AI? Whatever we want to create it to look like.
7. Adapting to Change: Prioritizing Mental Health, Data Analytics, and Community Care

The EMS industry continues to adapt to a rapidly changing landscape. In the coming year, we anticipate a growing focus on mental health support for EMS professionals, the integration of advanced data analytics for improved patient care, and the expansion of community paramedicine programs to bridge gaps in healthcare access. As challenges like staffing shortages and rising operational costs persist, innovative solutions and collaboration will be critical to ensuring we continue to provide high-quality emergency care.
8. Making EMS a Kitchen Table Issue in 2025

Last year, rising EMS costs, revenue, and solvency were the focus of my commentary.
To date, not much has changed.
Various EMS entities have lobbied state and local governments for many years with limited success and have achieved no cohesive national plan for a structured approach or sustainable funding because they have been barking up the wrong tree.
Lobbyists and advocacy groups are frankly out of time to continue bickering among themselves about minutia and pleading with policy makers whose main concern is unfunded mandates, task forces, focus groups and other red tape which only succeeds in preventing any money actually allocated to ever reach the local services or support the boots on the ground who are in dire need of help.
The priority for 2025 needs to be public education. Recruitment, staffing, salaries, funding, and clinical progression cannot happen without public support.
Tip O’Neil, the 47th speaker of the House of Representatives famously opined “All politics is local’”. Recognizing “People want to be heard” resulted in his losing only one election in over 50 years of public service.
This year’s election has proven that American voters have voiced their frustration at not being heard and demonstrated an enduring proclivity for voting in their self-interest- the cost of gas and eggs, freedom from fears real and imagined ranging from job security to physical safety- the kitchen table issues that directly affect them.
EMS needs to become a kitchen table issue by creating awareness at the local level.
The average American’s current interest and awareness of EMS can be described using an analogy: The flat tire: Didn’t think it would happen to them without warning. Believed their car had a safe spare, or did not want to invest the money for a product they might never need. The result? Limp down a dangerous road for the short term on a temporary donut, or potentially find that the trunk is empty, the AAA card is expired, and no one is coming to help.
Except not having EMS is more than an inconvenience-it can be a matter of life and death
Rural volunteer agencies, municipal services and for-profit mega ambulance corporations must accept the responsibility for educating the communities they serve on the role of EMS. They need to be transparent and realistic in describing their current capabilities and the options available to the community. Individual services must be prepared to explain how the EMS system works, the associated costs, and the risks associated with potential system failure. Providers who want their profession to become a thriving career field with opportunities for growth and salaries commiserate with the knowledge, risk, responsibility and essential nature of EMS need to stop complaining and do the work it takes to help make it happen.
Public perception studies consistently indicate that people recognize the importance of EMS and expect timely and effective emergency care, consider EMS an essential service, and are generally supportive of ensuring necessary funding. Voters, not politicians!
Ambiguous threats about the collapse of the system are unlikely to connect with the day-to-day interests of average Americans. Make it personal. Politicians understand that acting on issues that positively affect the voter’s lives are what keeps them in office.
Every agency should have an action plan for 2025 focused on making access to emergency service a personal issue for every individual in their response area. Being ubiquitous and relentless in pursuing opportunities to inform and involve the people you serve is the fastest way to turn the tide on sustainability. The rest can then follow.
9. AI-Driven Communication and Community Engagement in EMS

In 2025, one of the key trends we will see in EMS will be the rise of AI-powered crisis communication and real-time community engagement.
As EMS agencies face increasingly complex emergency situations, the ability to communicate quickly and effectively with the public will become even more critical. AI-driven tools and platforms will help EMS organizations automate and enhance their communication strategies, ensuring they provide timely updates during emergencies, manage public perceptions, and address community concerns.
Some ways this will manifest include:
- Real-time Social Media Monitoring and Engagement: EMS agencies will use AI to track social media and other digital platforms, identifying potential crises or public concerns in real-time. This will allow them to respond faster to misinformation, provide up-to-date information during major incidents, and engage with the community more effectively.
- Crisis Response Automation: EMS will increasingly rely on AI systems that can automatically send out pre-scripted responses to common questions during crises, minimizing delays and human error while ensuring clear and consistent messaging.
- Personalized Communication: Using data analytics, EMS providers will be able to target specific segments of the population with tailored messages, whether for public health campaigns, safety tips, or updates on ongoing emergencies. This personalization will improve community trust and engagement.
- Collaborative Platforms: EMS will integrate communication tools with local government agencies, law enforcement, and healthcare providers, enabling a unified and seamless flow of information during critical situations. This collaborative approach will not only ensure faster decision-making but also improve public perception of EMS as a part of a coordinated effort in community safety.
As these technological advances become more integrated, EMS agencies will become more adept at proactively managing their reputations, fostering stronger community ties, and ensuring public trust remains high in 2025 and beyond.
10. Embracing Technology to Mitigate the Effects of Inflation and Revenue Reductions in 2025

Although inflation may slow in the coming years, costs will continue to rise in 2025. A growing number of states have implemented Minimum Wage ordinances that are tied to automatic adjustment formulas based on changes in the consumer price indexes for their geographic areas.
Direct Labor costs are the highest cost line item on the balance sheet for most EMS organizations.
The incoming federal administration and congress have indicated a desire to reduce the federal deficit by cutting spending. Specifically, members of congress and the senate, have echoed the president-elect’s comments about finding savings at CMS in both the Medicare and Medicaid programs. This will no doubt result in revenue reductions or at a minimum, hamper revenue increase for many ambulance services throughout the country.
While in many other sectors automation is one method to reduce costs, in EMS, we are reliant on direct labor as a service industry. But we can employ technology to create efficiencies that result in savings to the bottom line!
Management teams should review all departments in their operations to assess where enhancements in the deployment of technology can reduce direct labor costs. Obvious places could include dispatch processes, billing tasks, quality assurance review, performance review, ePCR systems, data transfer, employee credentialing management, fleet management documentation, inventory management control, and so much more. The good news is there are plenty of high caliber vendors that support EMS organizations with high quality technology solutions tailored to our industry’s unique needs.
Whether your service is a two-ambulance fleet or a 1,000-ambulance fleet, in 2025, it will be crucial for all EMS organizations to review their systems to see what technologies are available to assist them to eliminate mundane tasks that their employees dread, and that will lower direct labor costs. In doing so, it might make both the crew and the accountant smile, at least for a little while!
About The Karras Group
Founded in 2005 and based in Mount Pleasant, Michigan, The Karras Group is a nationwide public safety consulting firm offering practical solutions for ambulance services, EMS organizations and related entities. To learn more about The Karras Group visit thekarrasgroup.com.
11. Data Remains Key

Organizations collect vast amounts of data during their daily operations. This data empowers them to operate more efficiently, meet regulatory standards, provide better service, enhance patient care, manage costs, and ultimately grow in a competitive landscape. In 2025, data-driven strategies will continue to foster improvement, adaptability, and innovation.
12. Cybersecurity Will Continue to Challenge EMS

A major trend I see is that there is a perfect storm brewing to challenge EMS organizations both economically and organizationally. First, you have Health insurance providers and government regulations squeezing transport provider revenue. Second, you have rising inflation increasing operational cost and staff stress levels. Finally, you have the unrelenting growth of cyberattacks aimed at extorting money from EMS organizations and disrupting business continuity because they are usually soft targets with valuable health data.
At Mamori.io we recognize that running an EMS organization is becoming increasingly challenging and stressful, and that is why we are focused on helping EMS organizations protect themselves from modern cyberattacks with a comprehensive, easy to deploy, and cost-effective all-in-one data security solution. Our mission is to remove the stress of cybersecurity from EMS business owners. Traumasoft is using Mamori.io to secure its valuable data, and we are happy to help all their partners and customers do the same. For small businesses under 20 users, we offer our comprehensive data security solution for free.
About Traumasoft
Traumasoft is one truly integrated product for Emergency Medical Services (EMS) that drives timely efficiencies. We are an all-in-one system capable of managing every aspect of your EMS operations. One system comprised of interconnected solutions handles staff, integrates processes, manages assets, and grows revenue. Schedule a demo today to see how we can help you increase operation efficiency and profitability.
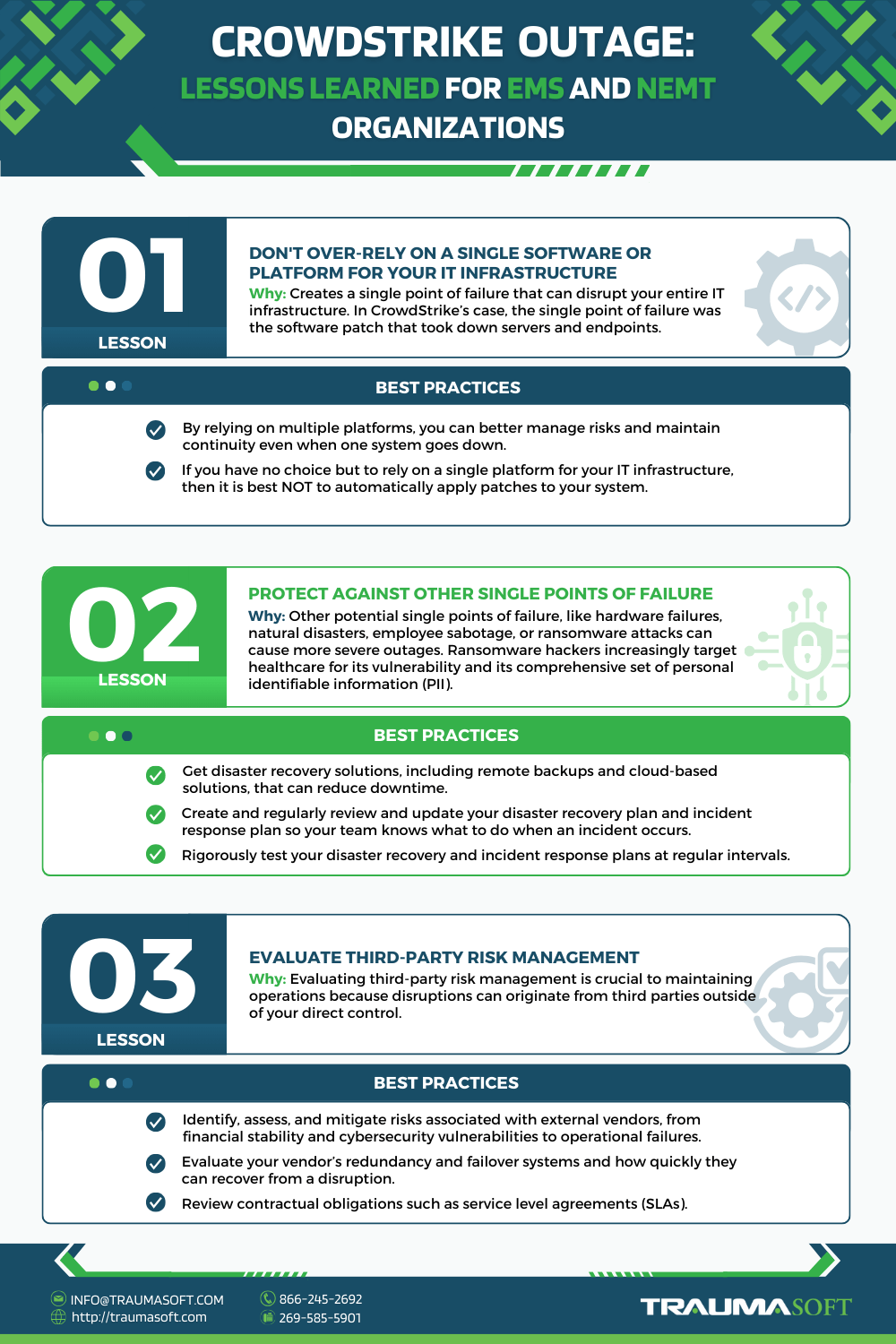
CrowdStrike Outage: Lessons Learned for EMS & NEMT Organizations and How to Mitigate

What happened with CrowdStrike should be a wake-up call for many EMS and NEMT organizations out there.
Boston EMS reverted to a system used 30 years ago because of the CrowdStrike outage.
Non-urgent medical visits were cancelled because of the outage at Massachusetts General Hospital.
Chatham EMS and Savannah Fire paramedics in Savannah, Georgia, had to switch from digital incident reports to pen and paper.
For life-saving services like EMS where every second counts, CrowdStrike’s incident highlights the importance of mitigating risks and single points of failure.
In this blog post, we’ll explore the key lessons learned from the CrowdStrike outage, focusing on how EMS and NEMT organizations can better prepare themselves and prevent similar unplanned downtime in the future.
A Quick Glance at the CrowdStrike Incident
In July 2024, CrowdStrike had a major outage that affected millions of computers around the world. The problem started when a software update (CrowdStrike Falcon) meant to improve security was automatically patched, causing many Windows systems to crash repeatedly. This led to what’s commonly known as the “blue screen of death”, where the computer shuts down suddenly and won’t start up properly.
The issue impacted critical services from hospitals, airlines, government agencies, and EMS/NEMT. Although a patch was released almost immediately to fix the error, many affected systems required manual repairs, making it a slow process to bring everything back to normal.
3 Lessons Learned for EMS and NEMT Organizations
Lesson 1: Try Not to Over-Rely on a Single Software or Platform for Your IT Infrastructure
The recent CrowdStrike outage highlighted the risks of over-reliance on a single platform in an IT infrastructure. When a critical issue has such widespread IT and operational exposure, it can create a single point of failure that disrupts entire operations. In CrowdStrike’s case, the single point of failure was the software patch that took down servers and endpoints.
This incident highlighted the need for organizations, especially those in essential services like healthcare and emergency response, to diversify their technology stack. By relying on multiple platforms and not putting all your eggs in one basket, you can better manage risks and maintain continuity even when one system goes down. While it may be challenging to switch endpoints away from Microsoft, migrating servers to alternative platforms should be considered.
Alternatively, if you have no choice but to rely on a single platform for your IT infrastructure, then it is best NOT to automatically apply patches to your system. Faulty patches manifest more frequently than what is released in the news. It’s always best process to test new patches in a pre-production, controlled environment before rolling them out to your IT infrastructure.
Lesson 2: Protecting Against Other Single Points of Failure
What happened in the CrowdStrike incident was a single point of failure caused by software. There are many other potential single points of failures that can cause more damaging outages, such as hardware failures, natural disasters, employee sabotage, or ransomware attacks. A few notable ransomware attacks include the MGM and Caesars ransomware attack and the CDK outage that affected more than 10,000 auto dealers. Ransomware hackers are increasingly targeting the healthcare industry because they are easy targets and house the most comprehensive set of Personal identifiable Information (PII).
To protect against other single points of failure mentioned earlier, you need well-planned disaster recovery strategies and solutions, including remote backups and cloud-based solutions that can reduce downtime. However, having a disaster recovery solution is not enough. You also need to have a disaster recovery plan and an incident response plan so your team knows what to do when an incident occurs. At the very least, both plans should outline the immediate step-by-step on what to do, including whom to communicate with and how to recover from each unique type of incident.
What’s more important is to rigorously test your disaster recovery and incident response plans. All too often, we see organizations letting their plans gather dust. When an incident does occur, the listed contacts in both plans have already left the company. The lack of testing is often what leads to an extended recovery time that results in significant losses.
Lesson 3: Evaluate Third-Party Risk Management
Many organizations rely on third-party vendors to operate, just as organizations today use CrowdStrike Falcon for cybersecurity. Evaluating third-party risk management is essential to ensure that your organization can maintain operations during disruptions, even when those disruptions originate outside your direct control.
Third-party risk management involves identifying, assessing, and mitigating risks associated with external vendors. These risks can include everything from financial instability and cybersecurity vulnerabilities to operational failures. When one of your critical vendors experiences an issue, it can have a ripple effect on your business, potentially leading to downtime, data breaches, or compliance violations.
When evaluating third-party risks, you should ask them questions like: Do you have redundancy and failover systems in place? How quickly can you recover from a disruption? You will also need to review contractual obligations such as service level agreements (SLAs) that specify acceptable level of downtime. To prevent over-reliance on a third party, develop a contingency plan that outlines how your organization will respond if a critical vendor experiences a disruption.
How to Mitigate: Using a Cloud-Based SaaS Solution
A well-established cloud-based SaaS solution like Traumasoft can mitigate the risks mentioned above.
Traumasoft is an all-in-one solution for EMS and NEMT organizations to manage their entire operations – from dispatch and ePCR to billing and reporting. Our solution is hosted in the cloud and can be accessed by simply launching a web browser.
At this point, you might be asking:
But… isn’t using Traumasoft’s all-in-one software relying on a single platform?
No, it is not because we rely on a diverse technology stack and multiple vendors so the risks are dispersed and mitigated. Traumasoft was NOT impacted by the CrowdStrike outage.
In essence, when you implement Traumasoft, you’re also getting the below technology stack:
A Diverse Technology Stack
Cloud-based SaaS solutions have been around since the early 2000’s, and Traumasoft has 16 years of experience and constant improvements to ensure that our diverse technology stack and infrastructure use proven best practices. We’re constantly evaluating third-party risk to prevent over-reliance on any third party or platform.
Disaster Recovery
Our platform is our bread and butter. That is why we have invested in disaster recovery, remote backups and recovery, and cloud-based backups and recovery. This is how we protect against single points of failure, including faulty software patches, hardware failures, employee sabotage, natural disasters, and other threats.
Cybersecurity and Data Security
We are well aware of the increasing cyberattacks on the healthcare industry, which is why we’ve implemented the zero-trust security model to protect against both internal and external threats.
Mobile, Tablet and Desktop Access via Web Browser
If you have a web browser, you can access Traumasoft for dispatch, ePCR, billing, and more. That means if your office PCs couldn’t boot because of CrowdStrike, your employees can improvise by using their home computers, tablets, or smartphone. You wouldn’t need to revert back to paper and pen like what happened to Boston EMS in the CrowdStrike outage.
Other Benefits of Using a Cloud-Based EMS and NEMT Solution
Virtual Offices and Remote Dispatchers
When work can be completed simply by using an internet browser, the employee can work anywhere, at any time. This makes virtual offices possible for office workers, such as dispatchers and billers. Several Traumasoft’s customers take advantage of this by employing remote dispatchers and/or billers to save on cost and improve employee retention.
Employee Retention
With a cloud-based SaaS solution, you can offer your employees the option to work from home and work more flexibly. Traumasoft takes employee retention further by lightening employee workloads through automation and by fostering camaraderie and collaboration with both web and mobile communication tools.
Lower Cost to Maintain
SaaS vendors like Traumasoft are responsible for monitoring, maintaining, and updating the infrastructure, ensuring that the software is always running at peak performance. The SaaS vendor carries the cost of hardware, software, and IT personnel, which is why this is can be such a cost-efficient option.
Scalability
As you grow, you only need to license for expanded usage. You do not have to worry about hardware capacity, IT workloads, or any other software costs.
Explore Traumasoft’s Technology Stack
At Traumasoft, we boast 99.9% uptime for our clients. Get a demo to explore our technology stack and see how we maintain this standard.
About Traumasoft
Traumasoft is one truly integrated product for Emergency Medical Services (EMS) and Non-Emergency Medical Transportation (NEMT) that drives timely efficiencies. We are an all-in-one system capable of managing every aspect of your EMS operations. One system comprised of interconnected solutions handles staff, integrates processes, manages assets, and grows revenue. Schedule a demo today to see how we can help you increase operation efficiency and profitability.
How to Improve EMS Billing and Get Paid Faster

Billing challenges are a common thorn in the side for many emergency medical service (EMS) providers. Issues like inaccurate documentation, coding errors, and delayed claim submissions can wreak havoc on an EMS organization’s financial stability. In practice, these problems can result in hundreds of millions of denied claims, and only a small fraction are likely to be appealed. Plus, billing problems don’t just strain resources and cut profitability; they also hinder healthcare providers from providing their patients with timely, effective, and life-saving care. It’s thus unquestionably in EMS providers’ best interest to invest in improved billing and revenue management.
Many modern EMS organizations have found success in this arena by adopting comprehensive solutions like Traumasoft. Overall, Traumasoft is a comprehensive software platform designed specifically for the emergency medical services industry. It offers a suite of integrated tools to help EMS organizations automate and manage various aspects of their operations, including billing. Such cutting-edge technology, supported by transparent communication practices and a well-trained staff, can streamline processes and alleviate many of the common headaches associated with revenue management in the EMS industry.
This article aims to highlight some key strategies for improving EMS billing and securing quicker payments. Your EMS organization can leverage the following practices to enhance operational efficiency and financial performance, thereby ensuring you can continue to provide high-quality emergency services while staying profitable:
Invest in Top-of-the-Line Billing Solutions
Efficient billing software is no longer a luxury but a necessity for EMS organizations seeking to stay competitive and productive in the digital age. Fortunately, the best billing solutions provide an immediate return on investment that can more than offset their upfront cost. The right software can all but eliminate manual errors and speed up claim processing times to transform your billing processes from the ground up.
Traumasoft’s advanced billing module offers features like automated coding, real-time claim status updates, and seamless integration with Traumasoft’s ePCR module. These capabilities keep your billing operations as smooth and accurate as possible so you face minimal risk of denied claims and delayed payments. Moreover, Traumasoft’s unified dataset eliminates data duplication and enhances the accuracy of your billing information. With Traumasoft in your corner, your company can unlock substantial efficiency gains that will ultimately lead to faster reimbursements and a more stable cash flow.
Ensure Documentation and Coding Are Accurate
Accurate documentation and coding are the backbone of a successful EMS billing process. Errors in these areas can lead to claim denials and delays that will severely impact your revenue cycle. It is thus imperative for your organization to capture all patient information thoroughly and accurately during encounters when filling out ePCR reports. Ideally, your ePCR software should have measures in place to guarantee correct coding and billing, you minimize the likelihood of errors that can disrupt the payment process.
Traumasoft’s ePCR module aids EMS professionals by providing a user-friendly interface for real-time data entry during patient encounters. It enables automatic data capture, and provides customizable templates where all necessary details can be recorded easily. The system supports thorough documentation through prompts and checks that guide EMS personnel in capturing comprehensive patient information accurately. What’s more, Traumasoft’s ePCR module is seamlessly integrated with the billing module, eliminating the need for double data-entry and the error associated with it.
Provide Continuous Education and Training for Staff
The EMS industry is continuously evolving, which means that your staff will also need periodic training to keep up with changes in the sector. Well-trained staff are better equipped to handle the complexities of EMS billing, from accurate documentation to proper claim submission. This expertise enhances efficiency and boosts the morale and confidence of your team, leading to a more productive work environment.
To support your team’s goal of continuous learning, Traumasoft provides various tools and resources that they can use to keep themselves knowledgeable and proficient in the latest EMS billing procedures. These include, but aren’t limited to, interactive training modules, up-to-date documentation on billing practices and regulatory changes, and access to webinars and online courses.
Conduct Regular Internal Audits and Reviews
Your organization will need to perform frequent financial audits and review to verify that your billing processes are operating up to speed. These audits help identify any inefficiencies or errors that could be costing your organization money and time. The benefits of performing them don’t just stop at compliance, either, as audits also help optimize your revenue cycle management. Scrutinizing your billing practices extensively can uncover patterns or recurring issues that need to be addressed so you can be assured that your processes are continually improving.
Streamline the Claim Submission Process
Your claim submission process needs to be as efficient as possible to secure timely payments. Implementing electronic claims submissions and stringent checks for accuracy and completeness can significantly reduce processing times and the likelihood of denials. Batch processing of claims (a feature that Traumasoft users love) and using automated reminders for follow-ups are other effective strategies to optimize the submission process. Implementing these practices ensures that your claims are submitted promptly and accurately, leading to faster reimbursements and improved cash flow.
Strengthen Communication with Both Patients and Payers
In addition to improving your operational processes and technological infrastructure, it’s equally important to work toward communicating clearly and transparently with both patients and payers. For patients, providing detailed billing statements and explaining their financial responsibilities can reduce confusion, disputes, and the manpower associated with them. You may also be able to facilitate quicker transactions by offering multiple payment options or setting up online portals for payments.
When dealing with payers, strive to establish strong relationships and maintain open communication channels, both of which can help you resolve issues more quickly. Address discrepancies or queries promptly to prevent delays in payment and iron out claims processing. Ultimately, prioritizing communication improvements will earn you benefits beyond financial ones, because doing so will also contribute to higher patient satisfaction and strengthen your rapport with insurance companies that you work with.
Utilize Reporting and Analytics Tools
Data analytics play a pivotal role in monitoring and enhancing billing performance. Your EMS organization can leverage analytics to track key performance indicators (KPIs) such as days in accounts receivable (AR), claim denial rates, and payment turnaround times, all of which are offered by Traumaosft’s EMS analytics module. These insights help identify bottlenecks and inefficiencies in the billing process, which then open up the opportunity for improvements.
Meanwhile, robust reporting tools enable your team to generate detailed reports that highlight trends and areas needing attention. Regularly review these reports so you have a realistic, up-to-date assessment of your billing operations. Plus, from a broader perspective, utilizing analytics and reporting also supports data-driven decision-making that can lead to better financial outcomes for your EMS organization.
Develop an Efficient Strategy for Denials and Appeals
No matter how much you optimize your billing processes, you will inevitably still have to deal with denials from time to time. An efficient denials management strategy starts with identifying common reasons for denials, such as incomplete documentation or coding errors, and training staff or implementing a solution like Traumasoft to avoid these pitfalls. A clear, systematic process for addressing and appealing denied claims can significantly reduce their impact. This includes timely follow-up on denials, utilizing tracking systems to monitor the status of appeals, and resubmitting claims with necessary corrections promptly.
It may also help to designate a dedicated team or individual to handle denied claims. This specialist should be well-versed in payer guidelines and adept at crafting compelling appeal letters. You can support the efforts of these individuals by reviewing the outcomes of your appeals and adjusting strategies accordingly. Your efforts in this area will likely further enhance the efficiency and success rate of your organization’s appeals process.
Observe Compliance with Regulations
EMS organizations must remain compliant with healthcare regulations and payer requirements to avoid penalties and facilitate smooth billing. Regulations frequently change, so you and your team will need to be proactive about keeping yourselves informed and adaptable. In addition to the regular training and financial audits mentioned above, implementing an EMS billing solution that checks your entries with rules and regulations (like what Traumasoft offers) can further enhance your organization’s ability to stay up-to-date with regulatory changes. This solution can track regulatory updates, automate compliance checks, and provide alerts for potential compliance issues.
There are naturally many benefits to adopting a proactive approach to compliance. Doing so helps your organization maintain a streamlined billing process, reduces the risk of costly errors, and preserves your good standing with regulatory bodies and payers. Overall, compliance both protects the organization from financial penalties and promotes a culture of accountability and continuous improvement internally.
Consider Outsourcing Billing Services
Some EMS organizations may find it more strategic to outsource EMS billing services, particularly those struggling with internal resource constraints. Specialized third-party billing companies possess the expertise and dedicated resources to handle complex billing tasks more effectively. These companies also stay current with industry regulations and technological advancements, so they can promise both seamless compliance and optimal performance.
Outsourcing can lead to faster claim processing, reduced administrative burden on staff, and improved overall financial health. And once they’ve tapped into the expertise of specialized billing services, EMS organizations can focus more on patient care and other critical functions. Additionally, outsourcing can provide greater scalability and flexibility, as EMS organizations have room to adapt to changing demands without overburdening their internal teams.
Improving your EMS billing process is not just about enhancing efficiency; it’s about securing the financial stability that allows your organization to thrive. Embracing the practices mentioned above positions your organization for better financial health and operational excellence. We at Traumasoft are more than happy to assist you in leveling up billing operations at your organization, so don’t hesitate to contact us today for a live demo on how our solution might serve your unique needs.
About Traumasoft
Traumasoft is one truly integrated product for Emergency Medical Services (EMS) and Non-Emergency Medical Transportation (NEMT) that drives timely efficiencies. We are an all-in-one system capable of managing every aspect of your EMS operations. One system comprised of interconnected solutions handles staff, integrates processes, manages assets, and grows revenue. Schedule a demo today to see how we can help you increase operation efficiency and profitability.